|
We‘ve all had those kids on our caseloads that just don’t progress very quickly in speech therapy…. it’s a puzzle, right?! I get questions nearly every day from SLPS with these “puzzles” and frequently my first question is, “what did the oral-facial exam reveal?”. More often than not, the answer is that one was never conducted. But, for kids with speech sound disorders, assessing the oral-facial mechanism is one of the most important, though frequently neglected, parts of a speech assessment. In fact, as outlined in ASHA’s Practice Portal regarding Speech Sound Disorders, an oral-facial examination (i.e., oral mechanism exam, oral peripheral exam, oral motor exam, etc.) is a key component of a comprehensive speech evaluation. Completing a thorough oral-facial exam (OFE) helps us as SLPs determine if the structure and/or function of the speech mechanism could be impacting speech production and frequently helps us identify that missing piece to those proverbial puzzles...  Sometimes it’s that child who you think is “just artic” but has this one sound they can’t seem to generalize into conversational speech. They may have a structural difference for which effortful compensations make it too difficult for carryover to take place.  Or that child who does fine on an articulation test but whose intelligibility is really reduced in connected speech and you just can’t put your finger on why. They may have motor planning deficits that a thorough OFE could help identify, such as how they perform on diadochokinetic tasks or volitional non-speech tasks.  Or maybe you just have a gut feeling that there’s “more going on” with a preschooler’s speech than a straight-forward phonological delay. They may also have some red-flags for myofunctional deficits, such as a high/narrow palate, mouth breathing, or a malocclusion, to which your OFE can alert you. A thorough OFE can help you uncover such contributors by looking at 2 aspects...  1. Structure Physical abnormalities may impact speech production, such as asymmetries, atypical dentition, the presence of dental appliances, abnormalities of the palate, like clefting or a bifid uvula, enlarged tonsils, or other unusual growths, just to name a few. If the actual structure of the oral mechanism is compromised then referrals to particular specialists (e.g., ENT, craniofacial team, neurologist, dentist, etc.) may be appropriate and therapy may need to focus on compensatory strategies.  2. Function OFEs can also uncover functional deficits by observing how each articulator performs on motor tasks to assess strength, range of motion, speed of movement, and whether or not extraneous movements or groping are observed during volitional motor tasks. These observations are key in helping us differentially diagnose dysarthrias and oral apraxia, as well as determining if targeted assessments are warranted, such as myofunctional or motor speech evaluations.  If you're a little intimidated by all the information you’re supposed to gather and interpret with an OFE, you’re not alone. It's why I spent so long developing my Oral-Facial Exam form... an easy to use 3-page exam form that includes additional pages of detailed instruction, guidelines, and diagrams to help any SLP feel confident administering and interpreting findings. But, if you feel like you need a little more guidance, check out my RESOURCES page where I've linked free webinars, podcast interviews, and video tutorials.... You may notice in all those courses and videos that I'm using my favorite OFE tools from Holland Healthcare... the Throat Scope and Telescope. They make administration SO. MUCH. EASIER. These light-up tongue depressors illuminate the oral cavity and help you see alllllll the things. The newer TelScope even allows you to capture intraoral images and videos for patient files and specialist referrals. And I haven't met a child that doesn't think it's a lightsaber or fairy wand. Bonus: You can purchase either device in an SLP Bundle along with my Oral-Facial Exam at a special price for SLPs. So, I hope I've managed to outline some of the benefits of administering a thorough OFE. If we haven’t identified or ruled-out underlying structural or functional issues, then we may be missing key information to help us make accurate diagnoses or make appropriate referrals to specialists, which means that we could also be wasting valuable time by using the wrong approach in therapy. Don’t let another child with a speech sound disorder be added to your caseload without doing an OFE… you never know how it may improve their trajectory in therapy.
5 Comments
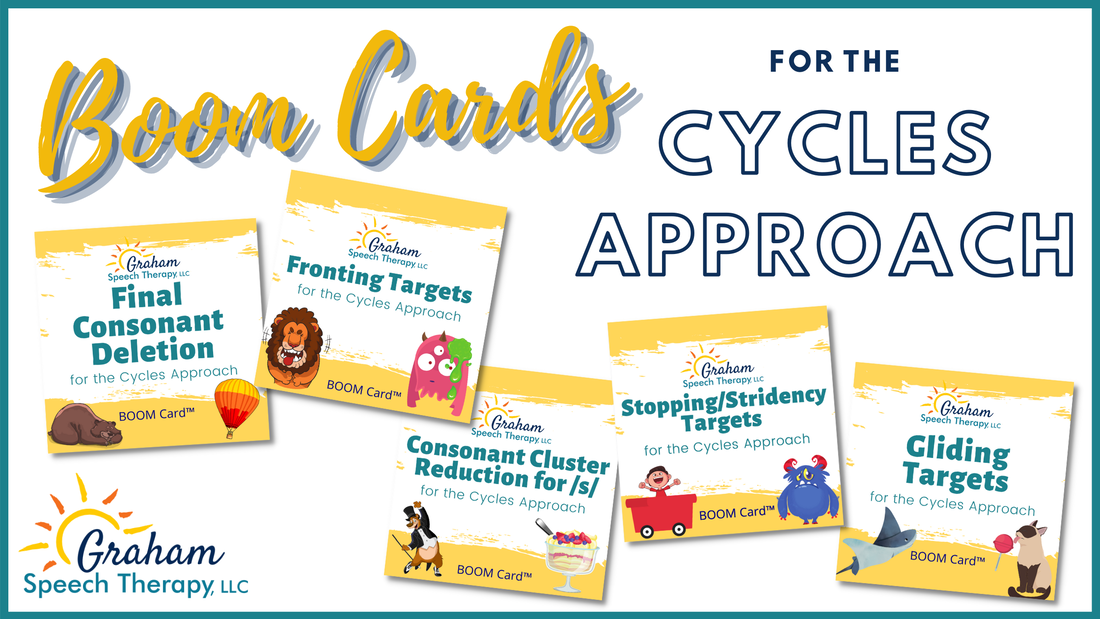
If you're new to Boom Cards, they're digital task cards accessed on the Boom Learning website. I learned about them when I had to switch to virtual therapy for all my clients following the pandemic and needed some engaging speech-specific activities to use over the computer. But, I quickly learned that this fun platform is great for in-person therapy, as well! One thing I found lacking, however, were activities that were intervention specific, when it came to my kids with phonological deficits. If you treat kids with speech sound disorders, you know that articulation resources are often not appropriate for phonological intervention (that's another post for another day!). So, I decided to make some "CYCLES" specific boom decks. What's great about these Cycles Boom Cards, is they actually make implementing cycles so much easier! Each deck includes all the components of a complete cycles session:
Here's a little video preview of one of my decks.... So, if you still don't feel super confident implementing the cycles approach, these Boom Cards can be a great resource. There are currently 5 decks addressing primary and secondary patterns, in alignment with cycles... with new decks being added regularly. You can find them on Boom Learning and Teachers Pay Teachers.
Want to know more about cycles? Watch this video I posted explaining it! Yup... I said it. Given all the buzz from that McCleod & Crowe article last year, it should be no secret that we've totally been misinterpreting those articulation norms. But, for a lot of SLPs it still begs the question... "then at what age should we be addressing particular sounds in speech therapy?"
Some of the most common questions I hear from SLPs sound something like this: "When should I start treating kids for /r/ errors?" ... or ... "Aren't /s/ sound errors still age appropriate for preschoolers?" Those are the WRONG QUESTIONS. If we base eligibility criteria and/or target selection primarily on arbitrary "cut-off" ages for acquisition of sounds, then we're missing the whole point. There are so many other variables that should be considered in addition to what particular sounds a child has at a particular age...
I like a good bar graph as much as the next guy... but I have to remind myself its just one piece of a bigger puzzle. Let's take the /s/ sound, for example. Here are some factors I take into consideration when I decide whether or not to recommend speech therapy:
Now, I completely understand that many school-based SLPs are all too often bound by black-and-white eligibility guidelines put in place by administrators with little to no understanding of the nuances of SSDs. And believe me, I can totally empathize with the concerns over gigantic caseloads in light of all these considerations (I was a school-based SLP for many years, myself). Unfortunately, I have no easy answers. I just know that we do our kids and their families a disservice when we solely rely on speech acquisition norms as an arbitrary threshold for eligibility criteria. With everything we’re learning about complexity theory, how we’ve been misinterpreting those speech acquisition charts, and how speech delays/disorders can impact literacy... it becomes pretty clear that there really is no “magic age” at which we should begin providing intervention for kids with errors of particular sounds. It’s much more complicated than that. |
|






 RSS Feed
RSS Feed